Karlo Tanjuakio is the Founder & Chairman at GLSS — a next-generation Business Process Efficiency platform.
In our increasingly complex healthcare system, ethical efficiency stands as a critical pillar to ensure patients receive quality care without unnecessary waste or unintended outcomes. Hospital systems play central roles in achieving this delicate balance. But how do we define ethical efficiency, and why does it matter?
What Is Ethical Efficiency?
Ethical efficiency is the principle of maximizing value—both in terms of outcomes and resource utilization—while adhering to moral and ethical standards. It is a philosophy I champion while helping leading companies around the world, including healthcare systems, increase their efficiency.
Ethical efficiency can measurably improve any industry, but it’s especially important in healthcare. In healthcare, it’s about creating a balanced system that upholds the highest ethical standards of care while driving productivity and impact for the greater good.
This involves:
• Ensuring fair access to care
• Minimizing waste in resources and processes
• Delivering patient-centered outcomes
• Promoting transparency and accountability
For hospital systems, the challenge lies in integrating these principles into operations, policies and decision-making processes. Let’s explore some key strategies for achieving ethical efficiency in hospital systems.
Focus On Nutrition As A Cornerstone Of Preventative Care
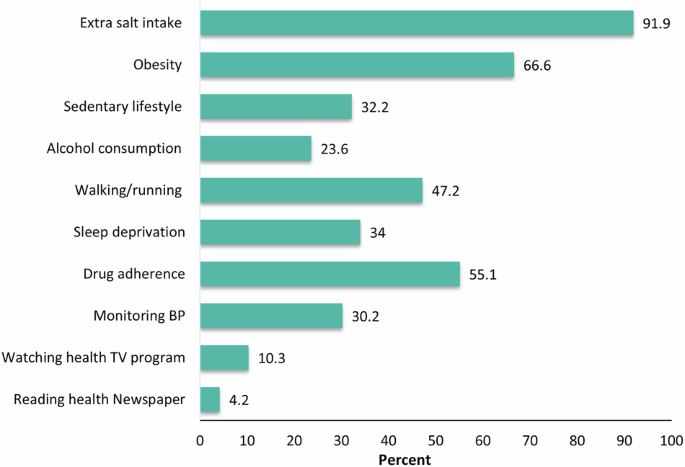
A staggering contradiction exists in U.S. healthcare: We spend more than any other nation on healthcare but rank poorly in outcomes and quality of life. Chronic diseases such as obesity, diabetes and heart disease—largely preventable through proper nutrition—cost our medical system more than $1 trillion each year.
The “food is medicine” mantra emphasizes that what we eat profoundly impacts our health and wellness. By incorporating this approach, healthcare can shift from reactive to preventative.
Dietary improvements can:
• Prevent and even reverse chronic conditions
• Enhance mental health and cognitive function
• Reduce reliance on medical interventions and medication
Hospital systems must recognize nutrition as a fundamental component of ethical efficiency. Programs such as medically tailored meal plans, nutrition counseling and community-based food initiatives have already demonstrated positive results.
Integrate Nutrition Into Hospital Systems And Clinics
Hospitals and clinics are ideally positioned to lead the charge in preventative care by:
• Providing wholesome meals to patients: Eliminate processed foods and incorporate nutrient-dense options into hospital menus to set an example for patients and staff.
• Launching community nutrition programs: Partner with local organizations to offer cooking classes, nutritional education and access to fresh produce to promote healthier lifestyles.
• Incorporating “food is medicine” into discharge planning: Patients recovering from illnesses often need structured guidance on how nutrition impacts recovery and long-term health.
Address Waste And Streamline Operations
Waste in healthcare is a well-documented issue. Hospitals can reduce waste by:
• Uncovering root causes: Sustainable and ethical improvements start with understanding the true sources of challenges—whether they stem from inefficiencies in patient care, rising costs or systemic barriers. By analyzing data and identifying these core issues, healthcare teams can implement targeted solutions that drive meaningful change.
• Reducing administrative redundancies: Healthcare organizations should find ways to simplify paperwork and approval processes to reduce delays in patient care.
• Improving patient flow management: Appointment scheduling and emergency room triage systems should be optimized to decrease wait times.
Shift To Value-Based Care Models
Shifting from fee-for-service to value-based care ensures that hospitals are incentivized to focus on patient outcomes rather than the volume of services provided. This model:
• Encourages preventative care and chronic disease management
• Aligns financial incentives with quality of care
• Reduces unnecessary tests and procedures
Foster A Culture Of Accountability
Ethical efficiency requires a strong organizational culture that prioritizes ethics. Hospitals must:
• Provide onboarding and compliance training: Programs that focus on ethical decision-making, process optimization and patient-centered care equip healthcare professionals with tools to navigate complex ethical dilemmas, fostering trust and accountability.
• Establish transparent policies: Clear guidelines on resource allocation and patient prioritization ensure fairness and positive outcomes.
Don’t Overprioritize Cost-Cutting At Patients’ Expense
Some hospital systems have implemented aggressive cost-cutting measures, such as understaffing critical units, which lead to compromised patient care. For instance, reducing nursing staff ratios to save costs often results in higher patient mortality rates and burnout among healthcare workers.
A Call For Ethical Efficiency In Healthcare
Ethical efficiency is not just a goal but a necessity for healthy, productive communities. As healthcare evolves and leaders improve their accountability and the Department of Government Efficiency searches for opportunities to reduce waste at the Centers for Medicare & Medicaid Services, healthcare organizations everywhere will likely follow suit and create patient-centered healthcare systems that balance profits with patient outcomes.
Together, we can create a healthier, more balanced future for everyone.
Forbes Coaches Council is an invitation-only community for leading business and career coaches. Do I qualify?
link